Abstract
Objective
The aim of this study was to assess the cost effectiveness of the novel fixed-dose anticoagulant rivaroxaban compared with the current standard of care, warfarin, for the prevention of stroke in patients with atrial fibrillation (AF).
Methods
A Markov model was constructed to model the costs and health outcomes of both treatments, potential adverse events, and resulting health states over 35 years. Analyses were based on a hypothetical cohort of 65-year-old patients with non-valvular AF at moderate to high risk of stroke. The main outcome measure was cost per quality-adjusted life-year (QALY) gained over the lifetime, and was assessed from the German Statutory Health Insurance (SHI) perspective. Costs and utility data were drawn from public data and the literature, while event probabilities were derived from both the literature and rivaroxaban’s pivotal ROCKET AF trial.
Results
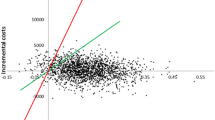
Stroke prophylaxis with rivaroxaban offers health improvements over warfarin treatment at additional cost. From the SHI perspective, at baseline the incremental cost-effectiveness ratio of rivaroxaban was €15,207 per QALY gained in 2014. The results were robust to changes in the majority of variables; however, they were sensitive to the price of rivaroxaban, the hazard ratios for stroke and intracranial hemorrhage, the time horizon, and the discount rate.
Conclusions
Our results showed that the substantially higher medication costs of rivaroxaban were offset by mitigating the shortcomings of warfarin, most notably frequent dose regulation and bleeding risk. Future health economic studies on novel oral anticoagulants should evaluate the cost effectiveness for secondary stroke prevention and, as clinical data from direct head-to-head comparisons become available, new anticoagulation therapies should be compared against each other.




Similar content being viewed by others
References
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 1991;22:983–8.
Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med. 1987;147:1561–4.
Go AS, Hylek EM, Phillips KA, et al. Prevalence of diagnosed atrial fibrillation in adults: national implications for rhythm management and stroke prevention: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. JAMA. 2001;285:2370–5.
Feinberg WM, Blackshear JL, Laupacis A, et al. Prevalence, age distribution, and gender of patients with atrial fibrillation. Arch Intern Med. 1995;155:469–73.
Kannel WB, Wolf PA, Benjamin EJ, et al. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol. 1998;82:2N–9N.
Hart RG. Warfarin in atrial fibrillation: underused in the elderly, often inappropriately used in the young. Heart. 1999;82:539–40.
Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007;146:857–67.
Bungard TJ, Ghali WA, Teo KK, et al. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000;160:41–6.
Gage BF, Eby C, Milligan PE, et al. Use of pharmacogenetics and clinical factors to predict the maintenance dose of warfarin. Thromb Haemost. 2004;91:87–94.
Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med. 2003;349:1019–26.
Levine MN, Raskob G, Landefeld S, et al. Hemorrhagic complications of anticoagulant treatment. Chest. 2001;119:108S–21S.
Kubitza D, Becka M, Roth A, et al. Dose-escalation study of the pharmacokinetics and pharmacodynamics of rivaroxaban in healthy elderly subjects. Curr Med Res Opin. 2008;24:2757–65.
Patel MR, Mahaffey KW, Garg J, et al. ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Red List Service GmbH. Red List 2012. Frankfurt am Main: German List of Pharmaceuticals; 2012.
Schwabe/Paffrath (Hrsg.). Arzneiverordnungs-report 2013. Berlin: Springer; 2013.
Kourlaba G, Maniadakis N, Andrikopoulos G, et al. Economic evaluation of rivaroxaban in stroke prevention for patients with atrial fibrillation in Greece. Cost Eff Resour Alloc. 2014;12(1):5.
Kleintjens J, Li X, Simoens S, et al. Cost-effectiveness of rivaroxaban versus warfarin for stroke prevention in atrial fibrillation in the Belgian healthcare setting. Pharmacoeconomics. 2013;31(10):909–18.
Rognoni C, Marchetti M, Quaglini S, et al. Apixaban, dabigatran, and rivaroxaban versus warfarin for stroke prevention in non-valvular atrial fibrillation: a cost-effectiveness analysis. Clin Drug Investig. 2014;34(1):9–17.
Morais J, Aguiar C, McLeod E, et al. Cost-effectiveness of rivaroxaban for stroke prevention in atrial fibrillation in the Portuguese setting. Rev Port Cardiol. 2014;33(9):535–44.
Lanitis T, Cotté FE, Gaudin AF, et al. Stroke prevention in patients with atrial fibrillation in France: comparative cost-effectiveness of new oral anticoagulants (apixaban, dabigatran, and rivaroxaban), warfarin, and aspirin. J Med Econ. 2014;17(8):587–98.
Lee S, Anglade MW, Pham D, et al. Cost-Effectiveness of rivaroxaban compared to warfarin for stroke prevention in atrial fibrillation. Am J Cardiol. 2012;110(6):845–51.
Harrington AR, Armstrong EP, Nolan PE Jr, et al. Cost-effectiveness of apixaban, dabigatran, rivaroxaban, and warfarin for stroke prevention in atrial fibrillation. Stroke. 2013;44(6):1676–81.
Coyle D, Coyle K, Cameron C, et al. Cost-effectiveness of new oral anticoagulants compared with warfarin in preventing stroke and other cardiovascular events in patients with atrial fibrillation. Value Health. 2013;16(4):498–506.
Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making. 1993;13:322–38.
Mueller S, Pfannkuche M, Breithardt G, et al. The quality of oral anticoagulation in general practice in patients with atrial fibrillation. Eur J Intern Med. 2014;25(3):247–54.
Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285:2864–70.
Camm AJ, Lip GY, De Caterina R, et al. 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association [published errata appear in Eur Heart J. 2013;34(10):790, and Eur Heart J. 2013;34(36):2850-1]. Eur Heart J. 2012;33(21):2719–47.
Earnshaw SR, Wilson M, Mauskopf J, et al. Model-based cost-effectiveness analyses for the treatment of acute stroke events: a review and summary of challenges. Value Health. 2009;12(4):507–20.
Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the panel on cost-effectiveness in health and medicine. JAMA. 1996;276:1253–8.
Weintraub WS. Pharmacoeconomic concepts in antiplatelet therapy: understanding cost-effectiveness analyses using clopidogrel as an example. J Cardiovasc Pharmacol Ther. 2008;13(2):107–19.
Federal Statistical Office of Germany. Life table for Germany. Wiesbaden; 2012.
Wyse DG, Love JC, Yao Q, et al. Atrial fibrillation: a risk factor for increased mortality: an AVID registry analysis. J Interv Card Electrophysiol. 2001;5:267–73.
Dennis MS, Burn JP, Sandercock PA, et al. Long-term survival after first-ever stroke: the Oxfordshire Community Stroke Project. Stroke. 1993;24:796–800.
Atrial Fibrillation Investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Arch Intern Med. 1994;154:1449–57.
Ariesen MJ, Claus SP, Rinkel GJ, et al. Risk factors for intracerebral hemorrhage in the general population: a systematic review. Stroke. 2003;34:2060–5.
Dodel RC, Haacke C, Zamzow K, et al. Resource utilization and costs of stroke unit care in Germany. Value Health. 2004;7(2):144–52.
Fang MC, Go AS, Chang Y, et al. Death and disability from warfarin-associated intracranial and extracranial hemorrhages. Am J Med. 2007;120(8):700–5.
Prencipe M, Culasso F, Rasura M, et al. Long-term prognosis after a minor stroke: 10-year mortality and major stroke recurrence rates in a hospital-based cohort. Stroke. 1998;29:126–32.
Atanassova PA, Chalakova NT, Dimitrov BD. Major vascular events after transient ischaemic attack and minor ischaemic stroke: post hoc modelling of incidence dynamics. Cerebrovasc Dis. 2008;25(3):225–33.
Passero S, Burgalassi L, D’Andrea P, et al. Recurrence of bleeding in patients with primary intracerebral hemorrhage. Stroke. 1995;26(7):1189–92.
Barinagarrementeria F. Patterns of recurrence of intracerebral hemorrhage. Semin Cerebrovasc Dis Stroke. 2005;5:168–71.
Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med. 1996;156:1829–36.
Tengs TO, Lin TH. A meta-analysis of quality-of-life estimates for stroke. Pharmacoeconomics. 2003;21:191–200.
Thomson R, Parkin D, Eccles M, et al. Decision analysis and guidelines for anticoagulant therapy to prevent stroke in patients with atrial fibrillation. Lancet. 2000;355:956–62.
O’Brien CL, Gage BF. Costs and effectiveness of ximelagatran for stroke prophylaxis in chronic atrial fibrillation. JAMA. 2005;293:699–706.
Gage BF, Cardinalli AB, Albers GW, et al. Cost-effectiveness of warfarin and aspirin for prophylaxis of stroke in patients with nonvalvular atrial fibrillation. JAMA. 1995;274(23):1839–45.
Gage BF, Fihn SD, White RH. Management and dosing of warfarin therapy. Am J Med. 2000;109:481–8.
The National Association of Statutory Health Insurance Physicians. Einheitlicher Bewertungsmaßstab (EBM), Stand: 4. Quartal 2012: Berlin; 2012.
Weimar C, Weber C, Wagner M, et al. Management patterns and healthcare use after intracerebral hemorrhage. A cost-of-illness study from a societal perspective in Germany. Cerebrovasc Dis. 2003;15(1–2):29–36.
Brüggenjürgen B, Diener HC, Berger AK, et al. Cost of atherothrombotic diseases—myocardial infarction, ischaemic stroke and peripheral arterial occlusive disease—in Germany. J Public Health. 2005;13:216–24.
Brüggenjürgen B, Rossnagel K, Roll S, et al. The impact of atrial fibrillation on the cost of stroke: the Berlin Acute Stroke Study. Value Health. 2007;10(2):137–43.
Winter Y, Wolfram C, Schaeg M, et al. Evaluation of costs and outcome in cardioembolic stroke or TIA. J Neurol. 2009;256(6):954–63.
Institute for the Hospital Remuneration System. G-DRG Fallpauschalenkatalog, Version 2012. http://www.g-drg.de/cms/Archiv/DRG_Systemjahr_2012_Datenjahr_2010#sm2.
German Social Code Book V—Statutory health insurance—§130a SGB V Rabatte der pharmazeutischen Unternehmer. http://www.sozialgesetzbuch-sgb.de/sgbv/130a.html.
Weinstein MC. Recent developments in decision-analytic modelling for economic evaluation. Pharmacoeconomics. 2006;24:1043–53.
Wallentin L, Yusuf S, Ezekowitz MD, et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: an analysis of the RE-LY trial. Lancet. 2010;376:975–83.
White HD, Gruber M, Feyzi J, et al. Comparison of outcomes among patients randomized to warfarin therapy according to anticoagulant control: results from SPORTIF III and V. Arch Intern Med. 2007;167:239–45.
Desbiens NA. Deciding on anticoagulating the oldest old with atrial fibrillation: insights from cost-effectiveness analysis. J Am Geriatr Soc. 2002;50(5):863–9.
Institute for quality and efficiency in health care. General Methods for the Assessment of the Relation of Benefits to Costs. Version 1.0. 2009.
National Association of Statutory Health Insurance Funds. Available from: http://www.gkv-spitzenverband.de/english/statutory_health_insurance/amnog___evaluation_of_new_pharmaceutical/amnog___evaluation_of_new_pharmaceutical_1.jsp. 2014.
Freeman JV, Zhu RP, Owens DK, et al. Cost-effectiveness of dabigatran compared with warfarin for stroke prevention in atrial fibrillation. Ann Intern Med. 2011;154(1):1–11.
Lee S, Mullin R, Blazawski J, Coleman CI. Cost-effectiveness of apixaban compared with warfarin for stroke prevention in atrial fibrillation. PLoS One. 2012;7(10):e47473.
Lip GY, Kongnakorn T, Phatak H, et al. Cost-effectiveness of apixaban versus other new oral anticoagulants for stroke prevention in atrial fibrillation. Clin Ther. 2014;36(2):192–210.e20.
Levy E, Gabriel S, Dinet J. The comparative medical costs of atherothrombotic disease in European countries. Pharmacoeconomics. 2003;21:651–9.
Kansal AR, Zheng Y, Pokora T, et al. Cost-effectiveness of new oral anticoagulants in the prevention of stroke in patients with atrial fibrillation. Best Pract Res Clin Haematol. 2013;26(2):225–37.
Kansal AR, Sorensen SV, Guni R, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in UK patients with atrial fibrillation. Heart. 2012;98:573–8.
Sorensen SV, Kansal AR, Connolly S, et al. Cost-effectiveness of dabigatran etexilate for the prevention of stroke and systemic embolism in atrial fibrillation: a Canadian payer perspective. Thromb Haemost. 2011;105:908–19.
Shah SV, Gage BF. Cost-effectiveness of dabigatran for stroke prophylaxis in atrial fibrillation. Circulation. 2011;123:2562–70.
Langkilde LK, Bergholdt Asmussen M, Overgaard M. Cost-effectiveness of dabigatran etexilate for stroke prevention in non-valvular atrial fibrillation. Applying RE-LY to clinical practice in Denmark. J Med Econ. 2012;15:695–703.
Mantha S, Ansell J. An indirect comparison of dabigatran, rivaroxaban and apixaban for atrial fibrillation. Thromb Haemost. 2012;108(3):476–84.
Waterman AD, Milligan PE, Bayer L, et al. Effect of warfarin nonadherence on control of the International Normalized Ratio. Am J Health Syst Pharm. 2004;61:1258–64.
Beyer-Westendorf J, Förster K, Pannach S, et al. Rates, management, and outcome of rivaroxaban bleeding in daily care: results from the Dresden NOAC registry. Blood. 2014;124(6):955–62.
Davis NJ, Billett HH, Cohen HW, et al. Impact of adherence, knowledge, and quality of life on anticoagulation control. Ann Pharmacother. 2005;39(4):632–6.
Dimberg I, Grzymala-Lubanski B, Hägerfelth A, et al. Computerised assistance for warfarin dosage: effects on treatment quality. Eur J Intern Med. 2012;23(8):742–4.
Eckman MH, Rosand J, Knudsen KA, et al. Can patients be anticoagulated after intracerebral hemorrhage? A decision analysis. Stroke. 2003;34:1710–6.
Olesen JB, Torp-Pedersen C, Hansen ML, et al. The value of the CHA2DS2-VASc score for refining stroke risk stratification in patients with atrial fibrillation with a CHADS2 score 0–1: a nationwide cohort study. Thromb Haemost. 2012;107:1172–9.
Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–100.
Bamford J, Sandercock P, Dennis M, et al. A prospective study of acute cerebrovascular disease in the community: the Oxfordshire Community Stroke Project: 1981–1986. 2. Incidence, case fatality rates and overall outcome at one year of cerebral infarction, primary intracerebral and subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1990;53:16–22.
Conflicts of Interest
The authors have no conflicts of interest to declare.
Author's contributions
Alexander Mensch developed the model, performed all analyses and drafted the manuscript. Stephanie Stock participated in drafting the manuscript and interpretation of the results. Björn Stollenwerk contributed to statistical analyses and interpretation of the results. Dirk Müller drafted the manuscript, conducted quality assurance and participated in the interpretation of the results. All authors read and approved the final manuscript. Alexander Mensch is the guarantor for the overall content.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Mensch, A., Stock, S., Stollenwerk, B. et al. Cost Effectiveness of Rivaroxaban for Stroke Prevention in German Patients with Atrial Fibrillation. PharmacoEconomics 33, 271–283 (2015). https://doi.org/10.1007/s40273-014-0236-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0236-9